A diagnosis of cancer is often followed by a deluge of medical terminology that can be overwhelming for patients and their families.
The question that immediately follows is: “What is the best treatment?” However, in modern oncology, there is no single “best” treatment. Cancer is not a monolithic entity; it is a heterogeneous collection of over 200 distinct diseases characterized by uncontrolled cellular proliferation.
Consequently, the answer to What Cancer Treatment is right for you depends on a complex interplay of histological grading, TNM staging (Tumor, Node, Metastasis), and increasingly, molecular profiling.
Historically, oncological protocols were somewhat linear—usually surgery followed by chemotherapy.
Today, we have entered the era of Precision Medicine. Treatment protocols are no longer just about the organ involved (e.g., “Breast Cancer”) but about the specific genetic mutations driving the malignancy (e.g., “HER2-positive Breast Cancer”).
This article provides a comprehensive, evidence-based overview of the current Modalities Of Cancer Therapy.
By understanding the mechanism of action behind these treatments, patients can better navigate the decision-making process with their multidisciplinary team.
Localized vs. Systemic Therapy: The Fundamental Classification
Defining the scope of intervention.
To understand Cancer Treatment Types, one must first understand the distinction between treating the site of the disease and treating the system of the patient.
In clinical practice, therapies are broadly categorized into two pillars:
A. Local Therapy

Local therapies are designed to treat a specific tumor or area of the body. They are typically used when the cancer is solid and confined to one location (non-metastatic).
- Goal: To achieve “Local Control”—physically removing or destroying the primary tumor mass.
- Modalities: Surgery and Radiation Therapy.
- Clinical Utility: These are often the primary curative modalities for early-stage solid tumors (e.g., Stage I/II Lung Cancer).
B. Systemic Therapy

Systemic therapies travel through the bloodstream to reach cancer cells throughout the body.
- Goal: To treat cancer that has spread (metastasized) or to eliminate microscopic disease that cannot be seen on scans (micro-metastases). This is also the primary treatment for hematological malignancies (blood cancers like Leukemia), where the disease is inherently systemic.
- Modalities: Chemotherapy, Immunotherapy, Targeted Therapy, and Hormone Therapy.
- Clinical Utility: These are critical for advanced stages or as “Adjuvant” therapy (given after surgery) to prevent recurrence.
This distinction is crucial because a patient may often require a Multimodal Approach—combining local therapy (to remove the bulk of the tumor) with systemic therapy (to clean up residual cells), a concept known as Oncological Treatment sequencing.
The Pillars of Local Therapy (Surgery & Radiation)
Targeting the tumor at its source.
For solid tumors (like breast, lung, or colon cancer), the primary objective is often “Local Control”—removing or destroying the visible mass.
A. Surgical Oncology: The “Gold Standard”

Surgery remains the oldest and most effective modality for curing solid tumors, provided the disease has not metastasized.
However, the intent of the surgery defines the procedure. It is not always about “curing” the patient; sometimes, it is about symptom management.
Understanding the surgical intent:
| Type of Surgery | The Clinical Goal | Example Scenario |
|---|---|---|
| Curative Resection | Complete removal of the tumor with “Negative Margins” (R0 Resection). The goal is to leave no cancer cells behind. | Removing a localized breast tumor (Lumpectomy) or a section of the colon (Colectomy). |
| Debulking (Cytoreduction) | Removing most of the tumor when complete removal is dangerous. This makes remaining cells more sensitive to chemo/radiation. | Common in Ovarian Cancer, where the surgeon removes as much visible disease as possible. |
| Palliative Surgery | Performed not to cure, but to relieve pain or restore function. | Removing a tumor blocking the intestine to allow the patient to eat, or stabilizing a spine fractured by bone metastasis. |
| Preventive (Prophylactic) | Removing an organ before cancer develops due to a high genetic risk. | Mastectomy for women with the BRCA1/2 gene mutation. |
We have moved away from “radical” surgeries (removing large amounts of healthy tissue) to Minimally Invasive Surgery (Laparoscopic and Robotic).
These techniques use smaller incisions, leading to faster recovery and less blood loss, which is crucial for initiating post-surgical treatments (adjuvant therapy) sooner.
B. Radiation Therapy (Radiotherapy)

Radiation therapy uses high-energy particles or waves (such as X-rays, gamma rays, or protons) to destroy or damage cancer cells.
Unlike surgery, which physically removes cells, radiation works at the molecular level. It uses Ionizing Radiation to cause “Double-Strand Breaks” in the cancer cell’s DNA.
Types of Radiation Delivery:
- External Beam Radiation Therapy (EBRT):
- How it works: A machine called a Linear Accelerator (LINAC) directs high-energy beams at the tumor from outside the body.
- Precision: Modern techniques like IMRT (Intensity-Modulated Radiation Therapy) allow oncologists to “sculpt” the beam to the shape of the tumor, sparing the heart and lungs.
- Brachytherapy (Internal Radiation):
- How it works: Radioactive sources (seeds, ribbons, or capsules) are placed inside the body, directly into or near the tumor.
- Advantage: This delivers a very high dose of radiation to a specific spot while protecting surrounding healthy organs.
- Common Use: Prostate cancer and Cervical cancer.
The Result: When the DNA is damaged, the cancer cell cannot replicate. It eventually dies (a process called Mitotic Catastrophe) and is flushed out by the body’s immune system.
Why it works: Cancer cells divide faster than normal cells and have poorer DNA repair mechanisms, making them more susceptible to radiation damage than healthy tissue.
The Pillars of Systemic Therapy (Chemo, Immuno, & Targeted)
Treating the whole system to prevent recurrence.
While local therapies address the visible tumor, Systemic Therapies are administered into the bloodstream to reach cancer cells that may have migrated to other organs.
These are the primary Therapies Of Cancer used to manage advanced disease and eradicate micro-metastases.
A. Chemotherapy: The Cytotoxic Approach
For decades, chemotherapy was the backbone of systemic treatment.
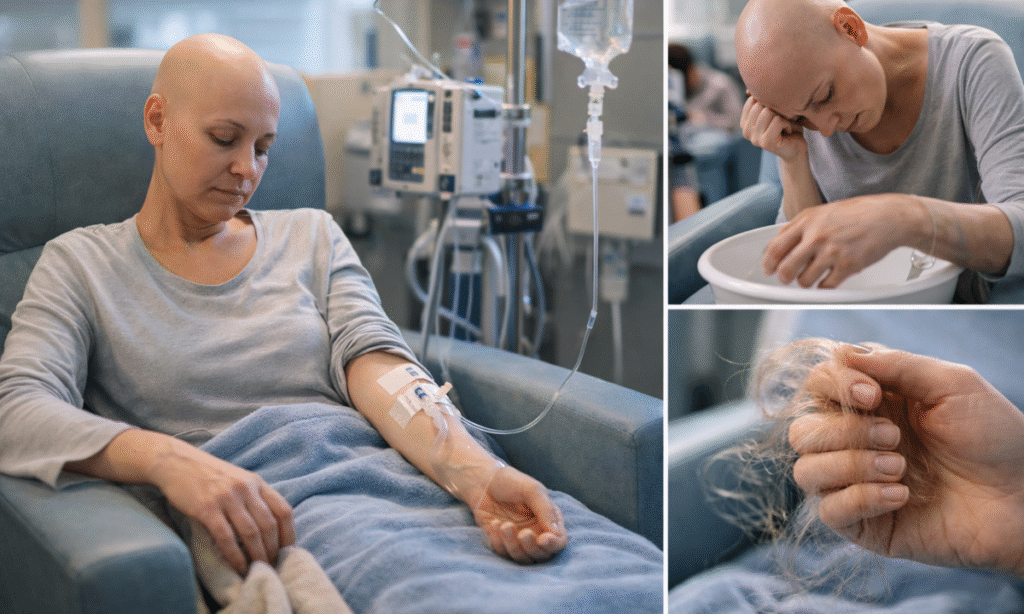
- Mechanism of Action: Chemotherapy drugs are “Cytotoxic” (cell-killing). They target cells that are in the process of dividing (Mitosis). Since cancer cells divide uncontrollably, they are the primary targets.
- The Limitation: Chemotherapy is not specific. It attacks any rapidly dividing cell in the body, including hair follicles, the lining of the gut, and bone marrow.
- Clinical Context: This “collateral damage” explains the classic side effects: hair loss (alopecia), nausea, and low immunity (neutropenia). Despite this, it remains highly effective for aggressive cancers like Leukemia and Lymphoma.
B. Targeted Therapy

Unlike chemotherapy, which acts like a grenade affecting a wide area, Targeted Therapy acts like a sniper rifle.
- Mechanism of Action: These drugs block the growth and spread of cancer by interfering with specific molecules (“molecular targets”) that are involved in the growth, progression, and spread of cancer.
- The Genetic Link: To use these, a patient must undergo genetic testing. For example, if a tumor has a mutation in the EGFR gene, an EGFR-inhibitor drug will shut down that specific growth signal.
- Clinical Success: This has revolutionized outcomes in difficult cancers. A prime example is cancer treatment for melanoma. Historically, metastatic melanoma had poor survival rates. Today, targeted therapies that inhibit the BRAF gene mutation have dramatically extended survival, turning a once-fatal diagnosis into a manageable chronic condition for many.
C. Immunotherapy
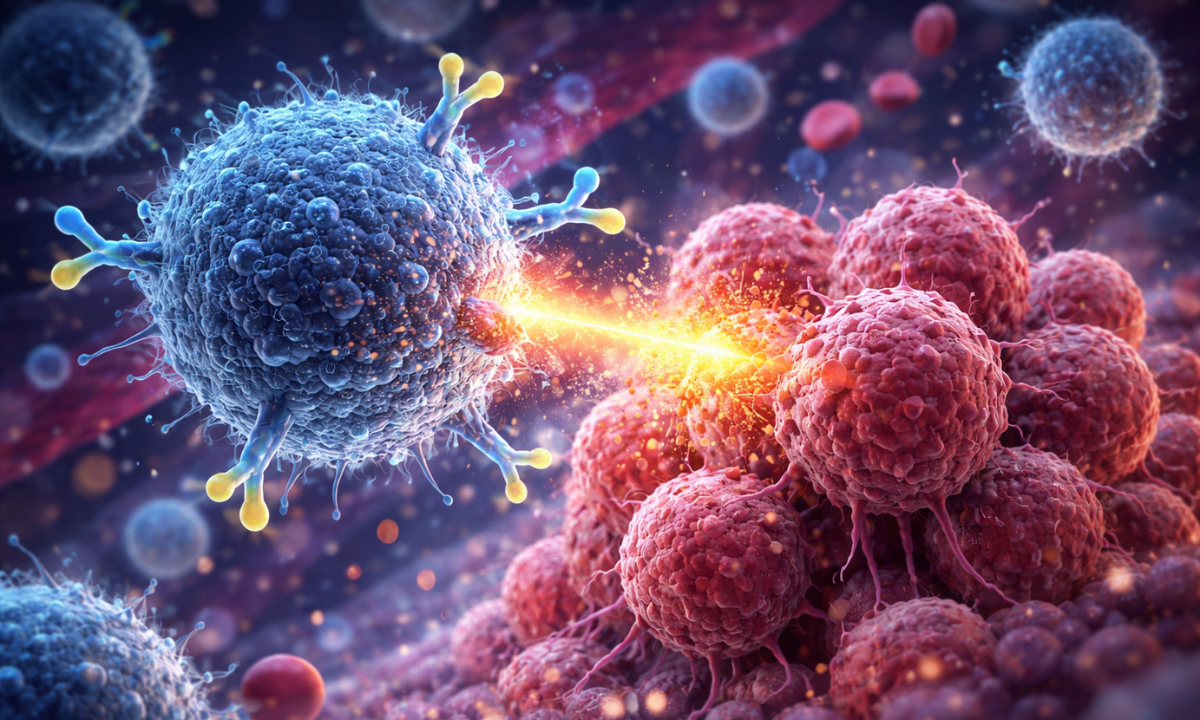
This is the newest and most promising pillar of oncology. Instead of attacking the cancer directly, it empowers the patient’s own immune system to do the job.
- The Problem: Cancer cells are masters of disguise. They often produce proteins (like PD-L1) that act as a “secret handshake,” telling the immune system, “I am a healthy cell, do not eat me.”
- Mechanism of Action (Checkpoint Inhibitors): Immunotherapy drugs (like Pembrolizumab or Nivolumab) block this secret handshake. They effectively “take the brakes off” the immune system, allowing T-Cells to recognize and destroy the cancer.
- Durability: Unlike chemo, where the cancer often grows back once the drug stops, immunotherapy can “train” the immune system to remember the cancer, leading to durable, long-term remission in some patients.
Summary of Systematic Modalities
| Modality | Target | Analogy | Best For |
|---|---|---|---|
| Chemotherapy | All rapidly dividing cells. | The Grenade: Powerful but causes collateral damage. | Fast-growing cancers; Adjuvant therapy. |
| Targeted Therapy | Specific gene mutations (e.g., EGFR, BRAF). | The Sniper: Hits only the bad cells, sparing healthy ones. | Cancers with identified mutations (Lung, Melanoma). |
| Immunotherapy | The Patient’s Immune System. | The General: Trains the army (T-Cells) to fight. | Cancers with high mutational burden: Lung, Kidney, Bladder. |
How is the decision made?

Precision Medicine requires collective intelligence.
Patients often ask, “Why did my friend get pills while I need IV chemotherapy for the same cancer?”
The answer lies in the specific biological fingerprint of your tumor. In modern Oncological Treatment, the decision of “What Cancer Treatment Is Right For You” is rarely made by a single doctor.
It is determined by a Multidisciplinary Tumor Board (MDT)—a meeting where Surgical Oncologists, Medical Oncologists, Radiation Oncologists, Pathologists, and Radiologists review your case together.
They analyze three critical factors:
- TNM Staging (The Anatomy):
- T (Tumor): Size and extent of the primary tumor.
- N (Nodes): Has it spread to nearby lymph nodes?
- M (Metastasis): Has it spread to distant organs?
- Rule of Thumb: Early stages (I & II) usually prioritize surgery/radiation. Advanced stages (III & IV) require systemic therapy.
- Histological Grading (The Aggression):
Pathologists look at cells under a microscope. “Low-grade” cells look almost normal and grow slowly. “High Grade” cells look disorganized and grow rapidly, often requiring aggressive chemotherapy.
- Biomarker Testing (The Genetics):
This is the new gold standard. Tests like Next-Generation Sequencing (NGS) scan the tumor’s DNA for mutations. If a specific driver mutation is found, the MDT may bypass chemo entirely in favor of Targeted Therapy.
Practical & Economic Considerations in India
Navigating the logistics of care.
While the science is global, the delivery of care is local. Understanding the cancer treatment cost in India is a vital part of the planning process for families.
- Cost Variance:
- Traditional Chemotherapy: Generally more affordable, ranging from ₹15,000 to ₹1 Lakh per cycle, depending on the generic drug availability.
- Immunotherapy: Represents the high end of the spectrum, often costing ₹1.5 Lakh to ₹4 Lakh per dose due to complex biologic manufacturing.
- Radiation: Costs vary significantly based on the technology (Linear Accelerator vs. CyberKnife).
- Insurance & Schemes: Most comprehensive health insurance policies cover Oncological Treatment, including day-care procedures for chemotherapy. However, “Oral Chemotherapy” (pills taken at home) sometimes faces coverage hurdles. Government schemes like Ayushman Bharat have also improved accessibility for basic surgical and chemotherapy protocols.
The Dasappa Advisory: Always ask your financial counselor for a “Cost-Benefit Analysis.” Sometimes, a more expensive surgery (Robotic) may result in a shorter hospital stay, ultimatelchmeoty costing the same as Open Surgery with a long recovery.
Choosing the Right Centre
Where technology meets empathy.
Selecting the right facility is as important as selecting the right drug. The best cancer hospital in Bangalore is defined not just by its building, but by its ecosystem.
Criteria for Selection:
1. Integrated Diagnostics: Does the centre have in-house PET-CT and Molecular Pathology? Time lost in sending samples to external labs can delay treatment initiation.
2. Linear Accelerator Capabilities: For radiation, precision is everything. Look for centres with Image-Guided Radiation Therapy (IGRT) to minimize side effects.
3. Nursing Expertise: Oncological nursing is a specialty. Chemo-ports and side-effect management require trained hands.
Conclusion
Cancer is no longer a singular battle; it is a managed journey involving sophisticated Modalities Of Cancer Therapy.
From the precision of robotic surgery to the intelligence of immunotherapy, the options have never been more effective.
The “right” treatment balances clinical efficacy with your Quality of Life.
If you are navigating a diagnosis and looking for a Cancer treatment hospital in Bangalore that offers world-class Multidisciplinary Tumor Board reviews, Dasappa connects you with the region’s leading oncological specialists.